Testosterone Replacement Therapy (TRT) has gained significant attention in recent years as more men recognize the impact of low testosterone (low-T) on their health and well-being. Testosterone is a crucial hormone responsible for maintaining muscle mass, energy levels, mood, and overall vitality. When levels drop due to aging or medical conditions, it can lead to fatigue, reduced libido, weight gain, and mental fog.
TRT is designed to restore testosterone levels to a healthy range, helping men regain their energy, confidence, and quality of life. However, while it offers many benefits, it’s important to understand who qualifies for treatment, the available options, potential risks, and how to begin the process safely.
In this guide, we’ll walk you through everything you need to know about TRT, including how to get tested, the different treatment methods, and essential factors to consider before starting therapy.
The Low-T Boom
In recent years, there has been a surge in awareness surrounding low testosterone, often referred to as Low-T. More men are recognizing the symptoms—fatigue, reduced muscle mass, low libido, and mood swings—and seeking medical solutions like Testosterone Replacement Therapy (TRT). This rise in demand is fueled by growing research, increased marketing of hormone therapies, and a shift in societal attitudes toward men’s health and aging.
According to studies, testosterone levels in men have been steadily declining over the past few decades. Research published in the Journal of Clinical Endocrinology & Metabolism found that average testosterone levels have dropped by about 1% per year since the 1980s. Additionally, a study in the Urology Times reported that nearly 40% of men over age 45 may have low testosterone, yet many go undiagnosed.
With more awareness and easier access to treatment, including TRT clinics, men are now exploring options to restore their hormonal balance. However, while TRT offers promising benefits, it’s crucial to understand its risks, eligibility criteria, and proper medical supervision before beginning treatment.
What is Testosterone Replacement Therapy?
Testosterone Replacement Therapy (TRT) is a medical treatment designed to restore testosterone levels in men experiencing low testosterone (Low-T). Testosterone is a vital hormone responsible for muscle growth, bone density, energy levels, mood regulation, and sexual health. When levels decline due to aging, medical conditions, or lifestyle factors, it can lead to symptoms such as fatigue, weight gain, depression, and reduced libido.
How Does TRT Work?
TRT replenishes testosterone in the body using various delivery methods, including:
Injections – Administered weekly or biweekly for a steady testosterone supply.
Gels & Creams – Applied to the skin daily, allowing testosterone absorption.
Patches – Worn on the skin to provide a continuous release of testosterone.
Pellets – Implanted under the skin for a slow, long-term release of testosterone.
Who Typically Seeks TRT?
Men who seek TRT often experience symptoms of Low-T, including:
✅ Chronic fatigue and low energy
✅ Decreased muscle mass and increased body fat
✅ Reduced sex drive and erectile dysfunction
✅ Mood changes, irritability, or depression
✅ Difficulty concentrating and brain fog
While TRT for Men can be life-changing for those with clinically diagnosed low T, it is not for everyone. A proper medical evaluation, including blood tests and symptom assessments, is essential before beginning treatment.
Can you get TRT online?
Obtaining TRT online has become increasingly accessible. Telemedicine platforms offer virtual consultations with licensed physicians, enabling remote diagnosis and prescription. However, caution is advised. Reputable providers require comprehensive blood tests and medical history review before prescribing. While convenient, online TRT should maintain the same medical standards as in-person treatment.
Pros of Online TRT
- Convenience
- Privacy
- Access to specialists
Cons of Online TRT
- Limited physical exam
- Potential misdiagnosis
- Quality concerns
How Are You Tested for Low Testosterone?
Testing for low testosterone (Low-T) involves a combination of symptom assessment and lab testing to ensure an accurate diagnosis. Since testosterone levels naturally fluctuate throughout the day, a proper evaluation requires multiple steps.
1. Symptom Review
A doctor will first assess your symptoms, which may include:
- Fatigue and low energy
- Decreased muscle mass and increased body fat
- Low libido and erectile dysfunction
- Mood swings, depression, or irritability
- Difficulty concentrating and memory issues
If these symptoms are consistent with Low-T, your doctor will order blood tests to confirm the diagnosis.
2. Blood Tests for Low Testosterone
A blood test is the most reliable way to measure testosterone levels. Doctors typically check for:
- Total Testosterone – Measures the overall testosterone in your bloodstream.
- Free Testosterone – The active form of testosterone available for use by the body.
- Luteinizing Hormone (LH) – Helps determine if the issue is due to testicular or pituitary gland dysfunction.
- Sex Hormone-Binding Globulin (SHBG) – Affects the amount of free testosterone available.
3. Timing Matters
Testosterone levels are highest in the morning, so tests are usually done between 7 AM and 10 AM for the most accurate results. If levels are low, your doctor may recommend a second test on a different day to confirm the diagnosis.
4. The Importance of Seeing a Qualified Doctor
It’s crucial to work with an experienced healthcare provider who specializes in hormone therapy. Self-diagnosing or using online-only tests without proper medical supervision can lead to misdiagnosis or unnecessary treatments. A doctor will consider your overall health, underlying conditions, and treatment options before recommending TRT.
Low Testosterone Causes
Low testosterone (Low-T) can be caused by a variety of factors, including aging, medical conditions, and lifestyle choices. Understanding these causes can help in managing and potentially preventing testosterone decline.
1. Aging
Testosterone levels naturally decrease with age. Starting around age 30, men experience a 1% decline in testosterone per year. By the time they reach their 40s and 50s, many begin to notice symptoms like fatigue, reduced muscle mass, and low libido. While this is a normal part of aging, some men experience a more rapid or severe decline, leading to the need for Testosterone Replacement Therapy (TRT).
2. Medical Conditions
Certain health conditions can significantly lower testosterone levels, including:
- Hypogonadism – A condition where the body produces little or no testosterone.
- Type 2 Diabetes – Studies show a strong link between diabetes and low T.
- Obesity – Excess body fat, especially around the abdomen, can lower testosterone levels.
- Chronic Illnesses – Kidney disease, liver disease, and autoimmune disorders can contribute to Low-T.
- Sleep Apnea – Poor sleep quality and sleep deprivation negatively affect testosterone production.
3. Lifestyle Factors
Unhealthy lifestyle habits can accelerate testosterone decline, including:
- Chronic Stress – High cortisol levels (the stress hormone) can suppress testosterone production.
- Poor Diet – A diet high in processed foods, sugars, and unhealthy fats can disrupt hormone balance.
- Lack of Exercise – Regular strength training and physical activity help maintain healthy testosterone levels, while a sedentary lifestyle can lower them.
- Alcohol & Drug Use – Excessive alcohol consumption and drug abuse can negatively impact testosterone production.
Addressing these factors through healthy lifestyle changes, medical intervention, and proper diagnosis can help restore testosterone levels and overall well-being.
Types of TRT Treatment Options
There are various testosterone replacement options, each suited to different needs. Each offers different benefits based on lifestyle, medical history, and convenience. The most common types of TRT include injections, gels, patches, pellets, and bioidentical hormone therapy. Choosing the right option depends on personal preference and a doctor’s recommendation.
1. Testosterone Injections (Shots)
✅ One of the oldest and most widely used TRT methods
✅ Administered intramuscularly or subcutaneously
How it works:
Testosterone shots deliver a direct dose of testosterone into the bloodstream via an injection. Depending on the specific type, injections can be self-administered at home or given by a healthcare provider (HCP).
Common injectable testosterone medications include:
- Depo-Testosterone (Testosterone Cypionate) – One of the most commonly used injections
- Aveed (Testosterone Undecanoate) – Requires less frequent injections (every 10 weeks after initial doses)
- Xyosted (Testosterone Enanthate) – Available as an autoinjector for easier administration but prescribed less frequently
Injection Frequency:
- Weekly to biweekly for most testosterone cypionate or enanthate injections
- Every 10 weeks for testosterone undecanoate (Aveed)
Pros:
✔️ Cost-effective compared to other TRT forms
✔️ Long-lasting results with fewer applications
✔️ Higher absorption rate compared to gels and patches
Cons:
❌ May cause fluctuations in testosterone levels between doses
❌ Some individuals experience pain or discomfort at the injection site
❌ Requires needles and proper administration training
2. Testosterone Gels
✅ Easy to use and non-invasive
✅ Applied directly to the skin for gradual absorption
How it works:
Testosterone gels are applied to areas like the shoulders, upper arms, or thighs and absorbed through the skin into the bloodstream. They provide a steady release of testosterone throughout the day.
Common brand-name testosterone gels include:
- AndroGel
- Fortesta
- Testim
- Vogelxo
Application Tips:
- Apply daily as per your doctor’s instructions
- Wash hands thoroughly after application
- Avoid skin contact with others to prevent accidental testosterone transfer
Pros:
✔️ Painless and easy to apply
✔️ Provides a consistent testosterone level
✔️ No needles required
Cons:
❌ Risk of accidental transfer to partners, children, or pets
❌ Requires daily application
❌ May cause skin irritation
3. Patches
✅ Daily transdermal testosterone delivery
✅ Mimics the body’s natural testosterone release
How it works:
A testosterone patch is applied to the skin, gradually releasing testosterone throughout the day. It offers a steady dose but requires daily replacement.
Pros:
✔️ No needles required
✔️ Provides consistent testosterone levels
Cons:
❌ Can cause skin irritation
❌ Not as commonly prescribed due to discomfort and visibility
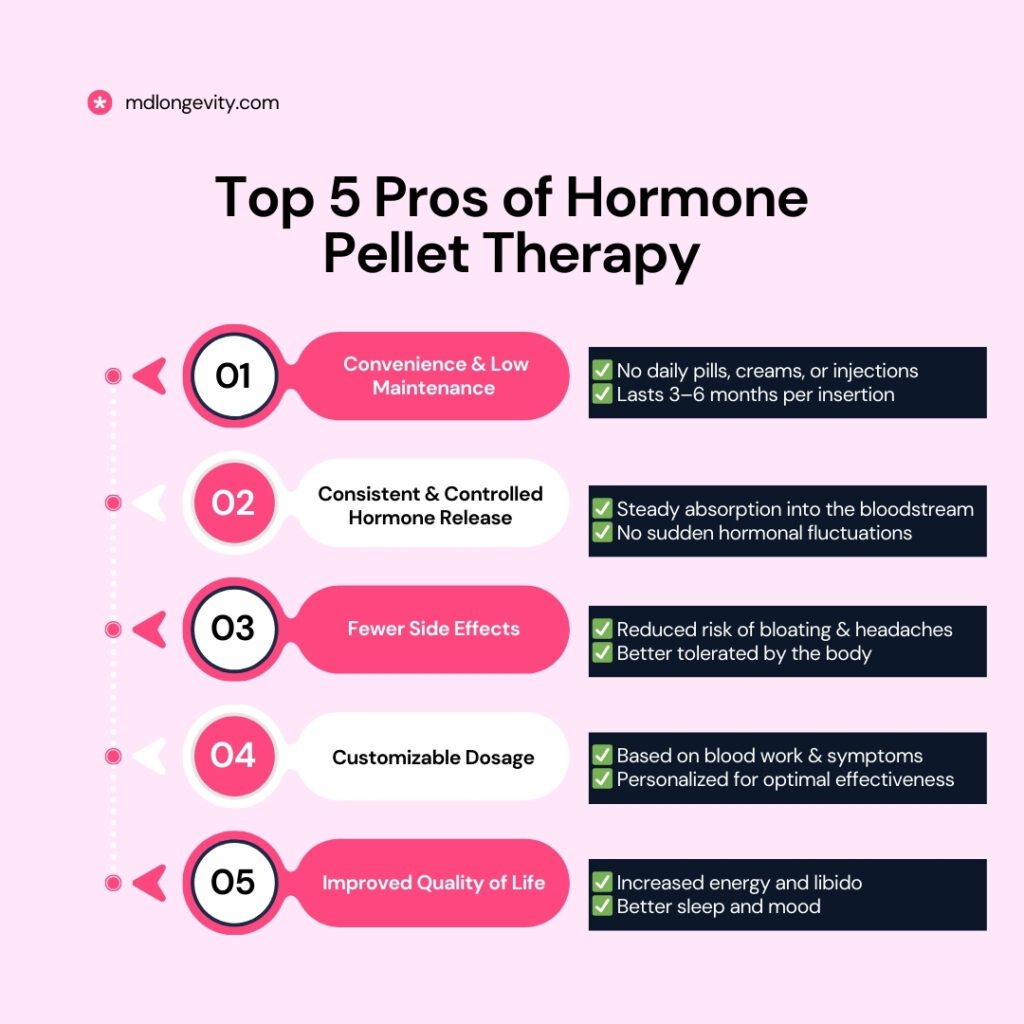
4. Pellets (Subcutaneous Implants)
✅ Long-term testosterone release (3–6 months)
✅ No daily maintenance required
How it works:
Testosterone pellets are implanted under the skin (typically in the hip or buttocks) through a minor surgical procedure. They slowly release testosterone over time, providing a consistent and long-lasting effect.
Pros:
✔️ No daily or weekly applications
✔️ Steady testosterone levels with minimal fluctuations
✔️ No risk of accidental transfer (unlike gels)
Cons:
❌ Requires a minor surgical procedure
❌ Difficult to adjust dosage once implanted
❌ More expensive than other options
5. Bioidentical Hormone Therapy
✅ Uses hormones identical to the body’s natural testosterone
✅ Can be customized for individual needs
How it works:
Bioidentical testosterone is derived from natural plant sources and is chemically identical to the testosterone produced in the body. It can be delivered in creams, gels, injections, patches, or pellets and is often tailored to each patient.
Pros:
✔️ Designed to closely mimic natural testosterone
✔️ Often seen as a more natural alternative
✔️ Can be personalized for dosage and delivery
Cons:
❌ Not always covered by insurance
❌ Requires frequent monitoring and dose adjustments
❌ Availability and regulation may vary by region.
Choosing the Right TRT Option
Each TRT method has unique benefits and drawbacks. The best choice depends on factors like personal preference, lifestyle, budget, and how well your body responds to treatment. Consulting a qualified doctor is essential to determine the most effective and safest TRT option for you.
What Are the Risks of Testosterone Therapy?
Testosterone Replacement Therapy (TRT) can provide significant benefits for men with low testosterone, but it is not without risks. While many men tolerate TRT well, some may experience side effects that range from mild to serious. Understanding these potential risks is essential before starting treatment.
Skin-Related Issues
One of the most common side effects of TRT is increased oil production in the skin, which can lead to acne. Some individuals may notice breakouts, particularly on the face, chest, or back. Oily skin can also contribute to clogged pores and irritation. This side effect is more likely in men who have a history of acne or naturally oily skin.
Increased Red Blood Cell Count
Testosterone therapy can stimulate red blood cell production, leading to a condition known as polycythemia. While red blood cells are crucial for oxygen transport, an excessive increase can thicken the blood, raising the risk of blood clots, stroke, or heart complications. Regular blood tests are necessary to monitor red blood cell levels and prevent potential complications.
Sleep Apnea and Breathing Problems
Men who already have sleep apnea may experience worsening symptoms after starting TRT. Testosterone can affect the way the brain regulates breathing during sleep, leading to interrupted breathing patterns. In some cases, TRT may even contribute to the development of sleep apnea in individuals who previously had no history of the condition. If sleep disturbances or excessive daytime fatigue occur, medical evaluation is necessary.
Impact on Fertility
One of the lesser-known effects of testosterone therapy is its potential to suppress sperm production. When the body receives testosterone externally, it can reduce natural testosterone production in the testes, leading to decreased sperm count and, in some cases, infertility. This effect is often reversible after discontinuing TRT, but men who plan to have children should discuss alternative treatments with a healthcare provider.
Fluid Retention and Swelling
Some men on TRT may experience fluid retention, leading to mild swelling in the ankles or feet. This side effect is usually temporary and resolves once the body adjusts to the therapy. However, men with pre-existing heart conditions or high blood pressure should be particularly cautious, as fluid retention can put additional strain on the cardiovascular system.
Potential Cardiovascular Risks
While research on the cardiovascular effects of TRT is ongoing, some studies suggest a potential link between testosterone therapy and an increased risk of heart disease, particularly in older men or those with pre-existing heart conditions. Monitoring cholesterol levels, blood pressure, and heart function is essential when undergoing long-term TRT.
Prostate Health Concerns
Testosterone has been linked to prostate growth, which can be a concern for men with an enlarged prostate (benign prostatic hyperplasia) or those at risk for prostate cancer. Although TRT does not directly cause prostate cancer, it may accelerate the growth of existing prostate cells. Regular prostate screenings are recommended for men receiving testosterone therapy, especially those over 50.
Mood and Behavioral Changes
Testosterone influences mood and energy levels, but for some individuals, TRT may lead to irritability, mood swings, or heightened aggression. While many men report improved well-being on TRT, others may experience psychological changes that require careful monitoring. Adjusting the dosage or exploring alternative therapies can help manage these effects.
Weighing the Risks and Benefits
Before starting TRT, it is crucial to assess individual risk factors and undergo a thorough medical evaluation. Regular monitoring, including blood tests and check-ups, helps ensure that any side effects are detected early and managed appropriately. While testosterone therapy can significantly improve the quality of life for men with low testosterone, it should always be approached with medical supervision and a clear understanding of potential risks.
Easy Energy Boosters (Before Considering TRT)
Before turning to Testosterone Replacement Therapy (TRT), making simple lifestyle changes can naturally enhance energy levels and support testosterone production. Many men experience low energy due to poor habits rather than medical conditions, and optimizing these factors can improve overall well-being.
Optimize Your Diet
What you eat has a significant impact on testosterone levels and overall energy. A balanced diet rich in essential nutrients can help the body maintain optimal hormone production.
- Protein: Supports muscle health and hormone balance. Good sources include lean meats, eggs, and fish.
- Healthy Fats: Essential for testosterone synthesis. Include sources like avocados, nuts, and olive oil.
- Zinc and Vitamin D: These nutrients play a key role in testosterone production. Oysters, spinach, and fortified dairy products are excellent sources.
Avoid processed foods, excess sugar, and alcohol, as they can contribute to energy crashes and hormonal imbalances.
Stay Active with Regular Exercise
Exercise is one of the most effective natural ways to boost testosterone levels and energy. Different types of workouts can provide unique benefits:
- Strength Training: Lifting weights has been shown to significantly increase testosterone levels, particularly when focusing on compound movements like squats and deadlifts.
- High-Intensity Interval Training (HIIT): Short bursts of intense activity followed by rest can help stimulate hormone production.
- Cardio in Moderation: While aerobic exercise improves heart health, excessive endurance training may reduce testosterone levels.
Consistency is key. Even a 30-minute workout a few times a week can improve energy levels and overall health.
Prioritize Quality Sleep
Sleep is essential for hormone regulation, and poor sleep can lead to lower testosterone levels and chronic fatigue.
- Aim for 7–9 hours of sleep per night.
- Maintain a consistent sleep schedule by going to bed and waking up at the same time daily.
- Reduce screen time before bed to minimize blue light exposure, which can interfere with melatonin production.
- Create a sleep-friendly environment with a cool, dark, and quiet room.
Good sleep habits can naturally restore energy levels and support overall hormonal balance.
Manage Stress Effectively
Chronic stress increases cortisol, a hormone that can suppress testosterone production and drain energy levels. Finding effective ways to manage stress is crucial for maintaining optimal hormone health.
- Practice Relaxation Techniques: Deep breathing, meditation, and mindfulness can help reduce stress levels.
- Stay Socially Connected: Spending time with family and friends can provide emotional support and improve mood.
- Engage in Hobbies: Doing activities you enjoy can help shift focus away from stressors.
Reducing stress not only improves testosterone levels but also enhances mental clarity and overall well-being.
A Natural First Step
Before considering TRT, focusing on diet, exercise, sleep, and stress management can significantly improve energy levels and hormone balance. These lifestyle changes are beneficial not only for testosterone production but also for long-term health and vitality. If symptoms persist despite making these adjustments, consulting a healthcare professional can help determine whether TRT is the right option.
Benefits of Testosterone Therapy
Testosterone Replacement Therapy (TRT) offers numerous benefits for men experiencing low testosterone levels. While results vary based on individual health and lifestyle factors, many men report noticeable improvements in energy, mood, and overall well-being.
Increased Energy and Muscle Mass
One of the most significant benefits of TRT is its ability to restore energy levels. Men with low testosterone often experience chronic fatigue and reduced stamina, making daily activities feel exhausting. With TRT, many regain their vitality, allowing them to stay active and productive throughout the day.
Additionally, testosterone plays a key role in muscle growth and maintenance. Low levels can lead to muscle loss and increased body fat. TRT helps:
- Improve muscle mass and strength, especially when combined with resistance training.
- Reduce body fat by enhancing metabolism and promoting lean muscle development.
- Increase endurance and physical performance, making workouts more effective.
Improved Mood and Mental Clarity
Testosterone is closely linked to mental well-being. Low levels can contribute to irritability, anxiety, and even depression. Many men on TRT report:
- A more positive mood and reduced feelings of stress.
- Improved mental focus and cognitive function, making it easier to concentrate and stay sharp.
- Greater motivation and overall confidence in daily life.
For those struggling with brain fog or difficulty making decisions, TRT can provide a clearer and more focused mindset.
Enhanced Libido and Overall Well-Being
Testosterone is essential for a healthy sex drive, and declining levels often lead to decreased libido and sexual performance issues. TRT can help:
- Restore a healthy sex drive and improve performance.
- Enhance overall sexual satisfaction and confidence.
- Improve overall well-being, helping men feel more youthful and engaged in life.
Many men on TRT report feeling more like themselves again, with a renewed sense of vitality and motivation.
A Personalized Approach to Treatment
While the benefits of TRT can be significant, results vary from person to person. A healthcare provider can help determine the right dosage and treatment plan based on individual needs. Regular monitoring ensures that the therapy is effective while minimizing potential risks.
Who Should Avoid TRT?
While Testosterone Replacement Therapy (TRT) offers significant benefits for men with low testosterone, it is not suitable for everyone. Certain health conditions and risk factors may make TRT unsafe or less effective. Before starting therapy, a thorough medical evaluation is essential to determine if TRT is the right choice.
Prostate Cancer History
Men with a history of prostate cancer or those at high risk should be cautious about TRT. Testosterone can stimulate prostate growth, potentially worsening pre-existing cancer. Although research is ongoing, most doctors recommend avoiding TRT if there is any history of:
- Active or previously treated prostate cancer.
- Elevated PSA (prostate-specific antigen) levels without a clear cause.
- A family history of aggressive prostate cancer.
Regular prostate screenings are necessary for men on TRT to monitor for any potential issues.
Severe Heart Conditions
Testosterone therapy may pose risks for men with pre-existing cardiovascular diseases. Some studies suggest that TRT could increase the likelihood of heart-related events in men with:
- Recent heart attack or stroke within the last six months.
- Severe hypertension (uncontrolled high blood pressure).
- Congestive heart failure (CHF) or other serious heart conditions.
Since testosterone can influence blood pressure and cholesterol levels, men with cardiovascular concerns should undergo careful monitoring before and during TRT.
High Red Blood Cell Count (Polycythemia)
Testosterone therapy can stimulate red blood cell production, which is beneficial in some cases but dangerous for men prone to polycythemia (excessive red blood cell count). This condition increases the risk of:
- Blood clots.
- Stroke.
- Deep vein thrombosis (DVT).
Doctors typically monitor hematocrit levels (a measure of red blood cells in the blood) during TRT. If levels become too high, treatment may need to be adjusted or discontinued.
Other Conditions to Consider
Men with the following conditions should also be cautious:
- Severe sleep apnea: TRT can worsen symptoms in some individuals.
- Liver or kidney disease: These conditions may affect how the body processes testosterone.
- Fertility concerns: TRT can suppress natural testosterone production, leading to reduced sperm count and infertility.
Taking a Cautious Approach to TRT
While Testosterone Replacement Therapy (TRT) can be beneficial for men with low testosterone, it’s important to approach treatment with a clear understanding of the potential risks and limitations. Before starting TRT, a thorough assessment and realistic expectations are essential.
Take Stock of Your Health First
Before considering TRT, evaluate your overall health, symptoms, and lifestyle. Many factors, including poor diet, lack of exercise, stress, and inadequate sleep, can contribute to low testosterone levels. Addressing these areas may naturally improve hormone balance. Common low-T symptoms to assess include:
- Persistent fatigue and low energy.
- Decreased libido and sexual performance issues.
- Loss of muscle mass and increased body fat.
- Mood changes, such as irritability or depression.
If these symptoms persist despite lifestyle changes, it may be time to seek professional evaluation.
Get an Accurate Assessment
TRT should only be started after a proper diagnosis from a qualified healthcare provider. A medical professional will:
- Conduct blood tests to measure testosterone levels at different times of the day.
- Review medical history to check for conditions that could mimic low testosterone.
- Assess overall health to determine if TRT is safe and appropriate.
A thorough assessment helps prevent unnecessary treatment and ensures TRT is the right option for you.
Be Mindful of the Possible Risks
While TRT can improve energy, mood, and overall well-being, it is not a one-size-fits-all solution. Potential risks include:
- Increased red blood cell count, which may lead to blood clot risks.
- Acne and oily skin due to hormonal changes.
- Worsening of conditions like sleep apnea or prostate issues.
- Suppression of natural testosterone production, potentially affecting fertility.
Understanding these risks allows for informed decision-making and proper monitoring throughout treatment.
Have Realistic Expectations
TRT is not an instant fix or a miracle cure. Results vary depending on individual health, age, and treatment adherence. Some men experience noticeable improvements within weeks, while others may take months. Realistic expectations include:
- Gradual increases in energy and mood stabilization.
- Improved muscle mass with consistent exercise and proper nutrition.
- Enhanced libido and sexual function over time.
Regular follow-ups with a healthcare provider ensure that TRT is working effectively and safely. By taking a cautious and informed approach, men can maximize the benefits of TRT while minimizing potential downsides.
Conclusion
TRT offers significant benefits for men with low testosterone, including increased energy and improved well-being. However, proper medical evaluation is essential before starting treatment, as natural boosters like diet and exercise may also help. Various options, such as injections, gels, and bioidentical hormones, provide flexibility, but potential risks must be considered.
A cautious, personalized approach ensures the best results with minimal side effects. Consulting a qualified provider for accurate diagnosis and monitoring is key. While TRT can be life-changing, it’s not a one-size-fits-all solution—realistic expectations and informed decisions are crucial for safe, effective treatment.
FAQs
- How can I get a testosterone prescription?
You need to visit a healthcare provider who will assess your symptoms and conduct blood tests to determine eligibility.
- What doctor prescribes testosterone?
Endocrinologists, urologists, and hormone specialists commonly prescribe testosterone therapy.
- What is the best way to get TRT?
The safest way is through a licensed physician after a proper diagnosis and lab testing.
- Can testosterone shots cause high blood pressure?
Testosterone injections may raise blood pressure in some individuals, so regular monitoring is important.
- How do I qualify for TRT?
Qualification depends on blood test results, symptoms, and a doctor’s evaluation.
- Is oral testosterone as effective as injections?
Injections are generally more effective and commonly prescribed, but oral forms are available for those who prefer them.
- How can I get testosterone legally?
The only legal way to obtain testosterone is through a licensed doctor’s prescription following a medical assessment.
Sources: